A recent article in the NY Times caught my eye. I couldn’t have agreed more, and also less. Titled “Let’s (Not) Get Physicals”, it was a reflection on the problems with conventional routine physical exams. http://www.nytimes.com/2012/06/03/sunday-review/lets-not-get-physicals.html?pagewanted=all
The time-honored tradition has been for a thoughtful patient to see her/his doctor for an annual exam. The article discussed several of the screening tests that have been the foundation of the annual exam routine. Many of these have been shown to be ineffective. Ineffective screening tests are worse than just a waste of time and money, as they lead to other needless tests and procedures. The procedures, the next steps looking to identify or treat the “disease” that is not there or does not need to be treated, usually create their own problems. The end result is that the patient has been harmed by this well-intentioned effort. Bear in mind that dumping procedural screenings is nothing new. Annual chest Xrays, anyone? We used to do that not so terribly long ago.
That was the agreeing part. My disagreement is based on the definition of what is done. From my experience it is certain that an appropriately directed annual health assessment is wise. That is true, even excluding the simple technology of a couple of blood tests. I see people every day who are so vitamin deficient that it shows up in simple blood tests from a conventional lab. But forgetting that, dumping all the post 19th century technology, there is ample, easily accessed and useful evidence of what needs to be changed to better a person’s health.
Taking to patients about how they feel, what they eat, their exercise patterns, how they are managing the stress of their lives, etc., tells me a lot. With that information, I can help them improve the quality of their day to day lives and avoid developing the most common diseases in our society (e.g., heart disease and diabetes). The risks of talking to a patient, looking over a three day diet record, reviewing his/her use of supplements/medications and conducting a simple physical exam are close to nothing.
Another shadow, looming over this discussion, is that doctors know that patients don’t change their habits. You can never get them (you) to change their diet or exercise. They won’t work to learn how to manage stress better. Docs know that. As you know very well, docs are wrong.
A child can learn to read and write without any help. but it will take a long, long time and incredible determination. When a doctor tells a patient that they should get more exercise, eat better, stop smoking or whatever, without providing the specific steps to achieve those formidable goals, almost no one is successful. The patient feels like a failure and the doctor’s negative expectations are confirmed.
What my colleagues do not know and what perpetuates this vicious cycle of hopelessness is HOW to help patients make changes. Medical school lasts four years. After that we have to get at least one year more of training, with most of us taking three or more. In all of that, there is little emphasis on the benefits of changing lifestyle and none on how to help patients make changes. When I earned a national level soccer coaching license I received some of my most valuable medical education. That was how I learned the nuts and bolts of helping people make changes. That has made a huge difference for me, and more importantly, for my patients.
If my colleagues were taught more about healthy lifestyle, low-tech examination and how to actually help patients make changes, annual exams would be powerfully positive health and life-enhancing experiences.
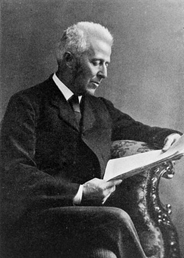
Who is that in the photo? It is Joseph Bell, MD. He was the inspiration for Sherlock Holmes. One of Conan Doyle’s medical school professor’s, Bell was renowned for his remarkable insight into his patients, based purely on his skills of observation and thoughtful deduction. He might be an even better model for physicians today than in his own time.
